
A few decades later, in 1863, Sir Thomas Richard Fraser wrote his thesis on the medicinal uses of physostigmine. Although small in size, its lethality was first discovered by Sir Robert Christison in 1855. Physostigmine originates from the Calabar bean, widely found in the African tropics, and is a highly toxic parasympathomimetic alkaloid. Physostigmine is a tertiary amine and a reversible cholinergic medication that was most commonly used to manage and treat antimuscarinic toxicity and glaucoma.

Summarize the multiple scenarios where physostigmine would be the drug of choice.Describe the effects of physostigmine on a patient presenting with antimuscarinic toxicity.Describe the effects of physostigmine on acetylcholinesterase.This activity will highlight the mechanism of action, adverse effects, dosing, monitoring, and relevant drug interactions necessary for members of interprofessional teams to make appropriate clinical decisions regarding patient care and their related conditions. Physostigmine originates from the Calabar bean, widely found in the African tropics. It is a tertiary amine and a reversible cholinergic medication most commonly used to manage and treat antimuscarinic toxicity and glaucoma. Physostigmine is a medication that was most commonly used to manage and treat antimuscarinic toxicity and glaucoma. With regard to neonatal myasthenia, Plauche related, "The onset of characteristic weakness in the infant may be delayed as long as 48 hours by coincident acquisition by the baby of anticholinesterase drugs given to the mother.". Neonatal myasthenia developed in several of the infants. None of the reports mentioned fetal or neonatal heart rates. Fetal anticholinesterase levels were not determined in any of these reports.
All eight patients underwent thymectomy, with improvement in their clinical condition. Eden and Gall presented eight case reports. Plauche presented three case reports and described current developments two of these patients received pyridostigmine. presented two case reports and reviewed the etiology, diagnosis, course, and treatment of pregnant patients with myasthenia gravis and who were receiving either neostigmine or pyridostigmine.
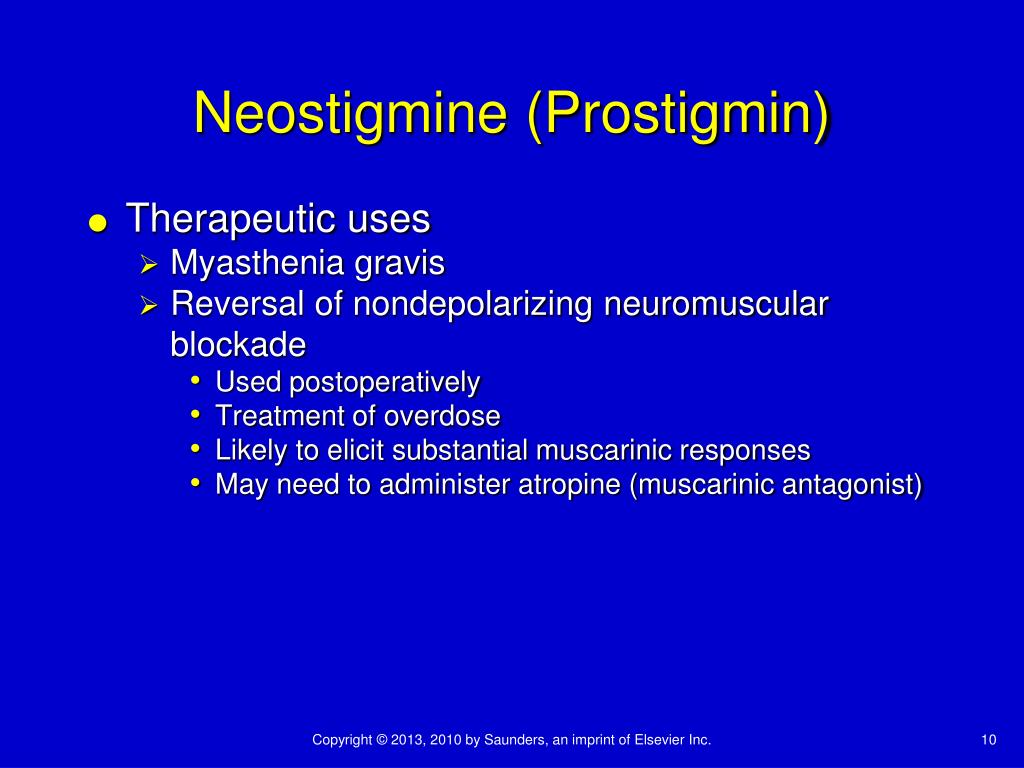
One of the patients received edrophonium, and another received neostigmine. McNall and Jafarnia presented five case reports and discussed management of labor and the postpartum period in patients with myasthenia. Most of the studies involving quaternary ammonium anticholinesterases in pregnancy involve patients suffering from myasthenia gravis. The patient awoke satisfactorily from the anesthetic without complication and delivered a healthy infant at term. At the end of the anesthetic, the muscle relaxant was antagonized with neostigmine (5 mg) and atropine (0.4 mg) intravenously. Fetal heart rate and uterine contractions were monitored, and left uterine displacement was performed. As before, general anesthesia was used along with vecuronium.
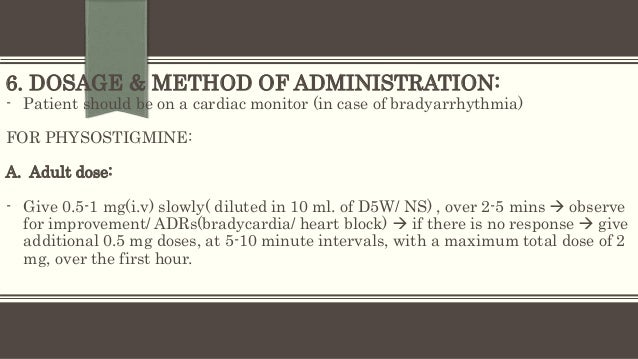
Four days postoperatively, however, the surgical repair was deemed unsatisfactory, and the patient underwent surgery. The rate eventually reached 130 beats/min after 1 h. Left uterine displacement was increased, and the fetal heart rate gradually returned to 120 beats/min. Fetal heart rate immediately decreased to the range of 90-110 beats/min after administration of neostigmine and glycopyrrolate. Preoperatively, the fetal heart rate was 153 beats/min but varied between 115 and 130 beats/min intraoperatively. Surgery proceeded satisfactorily, and the muscle relaxant effect was reversed at the termination of the anesthetic with neostigmine (5 mg) and glycopyrrolate (1 mg) intravenously. The fetal heart rate and uterine contractions were monitored externally during the procedure. Thiopental was used for induction of anesthesia, succinylcholine to facilitate intubation, and vecuronium to prevent patient movement during the operation. General endotracheal anesthesia was used (the patient would not cooperate for regional anesthesia) the primary anesthetics were isoflurane and nitrous oxide. She required open reduction of a fractured elbow. The patient was diagnosed as suffering from paranoid schizophrenia and was receiving haloperidol and lorazepam. The gestational age of the fetus was estimated to be 31 weeks. The patient was a 22-yr-old pregnant woman (gravida 1, para 0).


 0 kommentar(er)
0 kommentar(er)
